The antibiotics industry is in trouble. Operation Warp Speed may hold some solutions.
The antibiotics industry is in trouble. Operation Warp Speed may hold some solutions.
The rapid development of an effective COVID vaccine has been the main focus of the pharmaceutical industry for the last year and a half, for good reason.
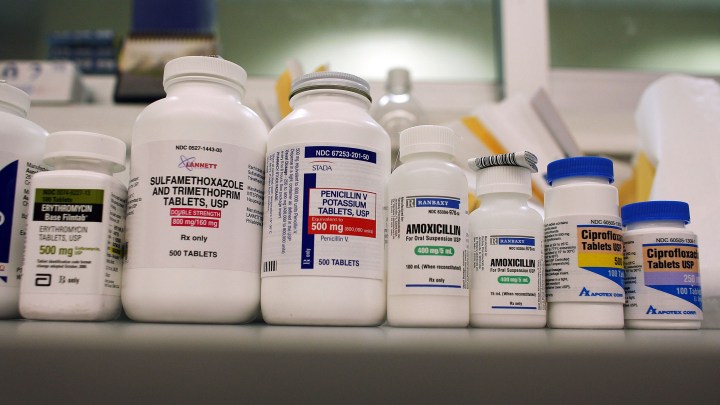
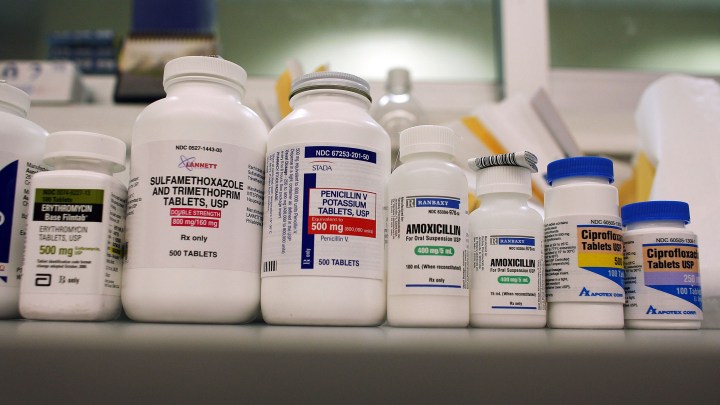
But another problem in the drug sector has been slowly building over the last 20 years — companies leaving or opting out of antibiotic drug development at a time when bacterial resistance is beginning to outpace development of new, stronger antibiotics.
This is largely due to the fact that antibiotics aren’t as lucrative as other drugs, which has led major pharma companies to leave the antibiotics sector, according to Maryn McKenna, journalist and senior fellow at the Center for the Study of Human Health at Emory University.
“Continuing to make antibiotics from the point of view of a pharmaceutical company has turned out to be something that’s just not sustainable,” McKenna said in an interview with “Marketplace Morning Report” host Sabri Ben-Achour.
The lack of big pharma companies in this space also means smaller biotech companies that have taken up the bulk of antibiotic development often become overwhelmed by the development cost, McKenna added.
Below is an edited transcript of the conversation on the antibiotics industry’s current condition and how Operation Warp Speed might provide new solutions to revitalize this sector of the pharmaceutical industry.
Sabri Ben-Achour: So first of all, to what extent are bacteria developing resistance to current antibiotics?
Maryn McKenna: Very widely. In fact, bacteria have been developing resistance to antibiotics for as long as we’ve had antibiotics, which is since the mid-1940s. We’ve always been able to stay ahead of their ability to develop resistance, resistance being basically their skill — if you can call it skill — at turning away the attack of antibiotics. But we’re losing ground on that.
The economics of antibiotics
Ben-Achour: So we are in this race with a class of deadly organisms. And yet, you have pointed out, all the big players who would make or develop new antibiotics left the business nearly 20 years ago. Why?
McKenna: It really does seem counterintuitive, doesn’t it? But if you think through the economics, there are good reasons for this. If you think back to the last time you took an antibiotic or a member of your family did, you probably didn’t take that drug for very long — a couple of weeks, maybe a month or two, if you were unlucky. It probably didn’t cost all that much money — a couple of hundred dollars at the most, maybe $1,000 or so if it was an IV drug instead of one you just swallow. And when you were done, that infection that you were taking the antibiotics for, should have gone away. All of those conditions are really different than most of the other drugs that pharmaceutical companies make and want to make money for. And as a result, continuing to make antibiotics, from the point of view of a pharmaceutical company, has turned out to be something that’s just not sustainable. Because the costs of making a drug — 10 to 15 years, at least a billion dollars — don’t actually vary by the category of drug that you’re making. But the amount of revenue that you get back at the far end of that is much greater if you’re making a cancer drug, an immunology drug, a drug for cardiovascular disease, than if you’re making an antibiotic.
Ben-Achour: You also talk about something called the “Valley of Death” problem when it comes to drug development, specifically for antibiotics. Can you explain that for us?

McKenna: Yeah, this is the tricky thing. So if you think through how a drug gets developed, most of us are kind of loosely familiar with that process. It starts out with an idea, with a compound, you do some preclinical work at a lab bench, then it goes into animal trials, then it goes into human trials, those phase one, phase two, phase three trials that people probably heard about in the past year in the context of the COVID vaccines. And then at the end of that you get to licensure by the FDA. When the very big pharma companies of the mid-20th century — we’re talking Pfizer and Eli Lilly and so forth — when they made antibiotics, they had multiple streams of income in their companies so that if their new antibiotic research was not making them any money yet and if it was costing them money, there was somewhere else in the budget that could help them pay for it. With those big companies with those multiple income streams having left the landscape, it falls to small biotechs, who have no other sources of income, except friends and family or maybe VC investors, to fund all of those phases of trials, some of which can be very large. And so it’s possible for them to run out of money before they get all the way to the end of the process to the FDA and get their drug approved.
A particular problem with antibiotics, which goes back to that issue of their just not being drugs that make a ton of money right away, is that there’s kind of a second “Valley of Death,” which is, after approval, but before a drug gets to profitability, enough to start making money to pay back all that R&D that the company put in. In the past couple of years, a number of those small biotechs that were making new drugs have gone bankrupt, put themselves up for auction, in various ways left the sector. And many of them did it after their drug had reached approval. So the economic landscape is super tricky, because there’s actually two sets of hurdles that a company with a needed, new drug has to get to before they can actually be confident that they can stay in the market for a while.
Incentivizing the production of antibiotics
Ben-Achour: So how do we fix this? How do we incentivize more production of antibiotics? And how do we make it financially possible?
McKenna: There’s a couple of sets of proposals that have been circulating over the past, almost a decade at this point. None of this gets created very quickly. Some of them are called “push incentives.” They push the drugs toward the point of approval. And some of them are called “pull incentives.” They pull the drug over that second “Valley of Death.” Push incentives have proved not too hard to accomplish. Basically, they are other forms of funding for that difficult research section that come from government or come from investment or come from varieties of private philanthropy that are getting these new drugs made by these small companies, sometimes with no other revenue streams, to the point where they can actually get their drug approved and put it on sale. The really challenging part that very few places, very few nations or jurisdictions, have managed, is that pull incentive: the point at which the drug ought to be able to go on sale, but still isn’t going to make enough money for years to keep that company afloat.
There’s one actually operating in the world at the moment, which is a program that was created less than a year ago by the government of the United Kingdom, that is kind of like a subscription model, sort of a zero coupon bond paid in drug where they give money to promising companies while their drug is moving through research on the guarantee that they, the government, with the National Health System, will get access to the drug afterward. And part of the point of incentives like that is not just a guaranteed income, but that the guaranteed income releases the pressure on the company to sell lots and lots and lots of the drug. Because with this underlying problem of resistance, the more you use a drug, the more bacteria learn what its attack mode is, the faster resistance will develop.
Ben-Achour: People pointed out in the past that the economics of developing vaccines was similarly fraught. And yet we managed to make it work and make it work very quickly for COVID. Did we learn anything from that that could be applied to antibiotics?
McKenna: You know, over the past 18 months as COVID responses were being worked on, I periodically talked to antibiotic developers. And what I kept hearing from them was intense envy at all the things that were being done to get COVID vaccines and therapeutics out to the market. There were changes in financing. Operation Warp Speed, the big investment by the U.S. government, was $18 billion. It just paved over those “Valleys of Death” that we just talked about. But there also were changes in how clinical trials were structured, the way in which the [Food and Drug Administration] staff was willing to talk to companies as clinical trials were going through. There were guarantees of purchase at the far end, there were a whole bunch of things that just flattened the various hurdles that would keep a drug from getting to market. And that was appropriate, right? Because COVID has been the worst public health challenge in more than 100 years. The people who develop antibiotics say, “Look, resistance is really serious. At some point we are going to face something like this, we should consider this kind of making the landscape easier for new antibiotics as well, so that we have them in time when we need them.”
There’s a lot happening in the world. Through it all, Marketplace is here for you.
You rely on Marketplace to break down the world’s events and tell you how it affects you in a fact-based, approachable way. We rely on your financial support to keep making that possible.
Your donation today powers the independent journalism that you rely on. For just $5/month, you can help sustain Marketplace so we can keep reporting on the things that matter to you.


















