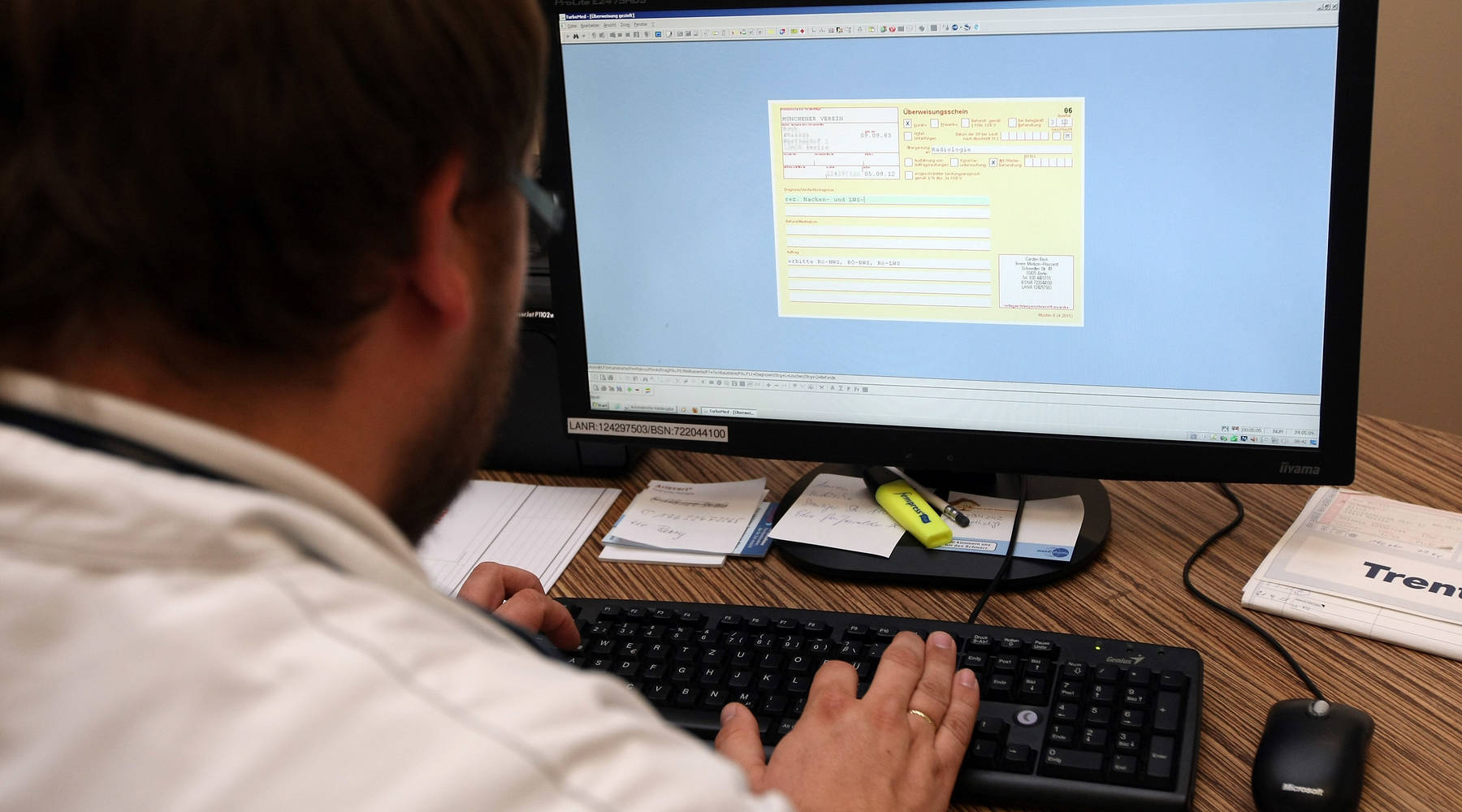
The pandemic is putting electronic medical records to the test

To slow the spread of the coronavirus, testing is essential — and not just getting a test, but getting the results back as quickly as possible. A recent survey found that the average wait time for results is four days, with 10% of the people surveyed waiting 10 days or more.
A shortage of the equipment and chemicals needed to perform the tests is part of the problem, but the country also lacks a robust electronic medical record system, which would allow information to be shared seamlessly.
I spoke with Julia Adler-Milstein, a professor of medicine at the University of California, San Francisco, where her research focuses on electronic health records. I asked her if part of the problem is all the different software providers — companies like Epic, CareCloud and Athenahealth — not playing nicely together. The following is an edited transcript of our conversation.

Julia Adler-Milstein: I do think there’s a roadblock there. I mean, that’s really been an Achilles’ heel of the past decade where we’ve seen so much more digitization of health information, but not as much of an effort put on making sure that that information can move around seamlessly where it’s needed. And I think in an ideal world, yes, those large companies would have cooperated and figured out how to build their systems in a way that were more compatible. But we also didn’t really create strong incentives for them to do that, and now we’re working to try to correct that. I think COVID-19 has shone a really bright spotlight on the need to do that. But it wasn’t there from the start, and I think we’re really paying the price for that now.
Amy Scott: What about privacy concerns with information being shared more widely in more places? I wonder if patients opting out may be part of the hurdle here.
Adler-Milstein: It is, and privacy concerns go hand in hand with greater ability to move and share information, because you want to be sure that it does end up in the right hands and not the wrong hands, and that the patients are involved in that in the way that is appropriate. I think one of the issues that is hard to know is in what level of detail or granularity does a patient want to be involved in managing who sees their information and for what purposes? And to do that at scale is really hard, because we know different people have different preferences overall and for specific types of information … what they might want to share with their health insurer versus their doctor. So it gets very complex very quickly. So I think everyone agrees we should have the privacy protection, but actually implementing that privacy protection and control is where it gets pretty complicated.
Scott: I’m also wondering about the cost of all this. I know the federal government has already spent tens of billions of dollars to encourage the adoption of electronic medical records. Do you have a sense of the price tag on what this effort could cost to get it right?
Adler-Milstein: I don’t think we’ve really seen good cost estimates, because part of it is sort of what we are paying for. I don’t think at this point we’re really paying for the infrastructure. This is really about linking up all of the digital entities and writing down rules of the road. I don’t think anyone really has a sense of the price tag. My personal sense is that it would be lower than the investment that we’ve made so far, because there’s so much cost in just the digitization itself. But there’s also some real costs in trying to figure out how to make all the different systems talk to each other.
Scott: But potentially lots of savings, too, I imagine?
Adler-Milstein: Oh, absolutely. There have been some estimates of that, and they’ve been in the $70 billion to $80 billion a year of potential savings if we really were to get to fully standardized seamless information sharing. The fact that hospitals are filling out spreadsheets with their COVID-19 testing data and sending it to the federal government —it’s staggering to think that we’re still doing that in the year 2020. But then also to think about all the costs of all the people in those hospitals who are manually entering data into a spreadsheet. It’s sort of hard to believe.
Scott: Yeah, and if I never have to try to remember when my knee surgery was when I see a new doctor, it’ll be too soon. How many of those health questionnaires have we all filled out again and again?
Adler-Milstein: Yeah. On the patient side, exactly. I mean, we haven’t even addressed those costs. Also, I think the stress that we put on patients when it’s clear that their doctor doesn’t know their medical history. If you were to show up today and tell your doctor that you’ve had a COVID-19 test and then for that doctor to say, “Oh, well, I don’t have any way to access that information,” that is not delivering patient-centered care.
Related links: More insight from Amy Scott
Another wrinkle in all this: Just because your test results are in the system, doesn’t mean your doctor will see them right away. These are busy people with lots of patients counting on them. Adler-Milstein said that so far the solution is just pinging doctors with lots of alerts, which if you’ve ever had to mute a group text chat, you know it can create notification fatigue.
While most hospitals now have some kind of electronic health records system, public health departments are still far behind, relying on phones and even fax machines to share information. That’s the subject of an episode of the health podcast “Tradeoffs” from my former Marketplace colleague Dan Gorenstein. Molly Wood had him on this show in May. Dan found that technology and data gaps keep public health officials dangerously out of the loop as they fight the spread of coronavirus.
A survey from the Pew Charitable Trusts found that most Americans support efforts to improve how medical records are shared between providers but have significant concerns about privacy and accuracy. And respondents were generally less comfortable with the sharing of sensitive information, like substance use, mental health issues and homelessness —factors that can influence health, but also potentially how patients are treated.
The future of this podcast starts with you.
Every day, the “Marketplace Tech” team demystifies the digital economy with stories that explore more than just Big Tech. We’re committed to covering topics that matter to you and the world around us, diving deep into how technology intersects with climate change, inequity, and disinformation.
As part of a nonprofit newsroom, we’re counting on listeners like you to keep this public service paywall-free and available to all.
Support “Marketplace Tech” in any amount today and become a partner in our mission.