Fever-screening devices used in many places are not helping control the pandemic
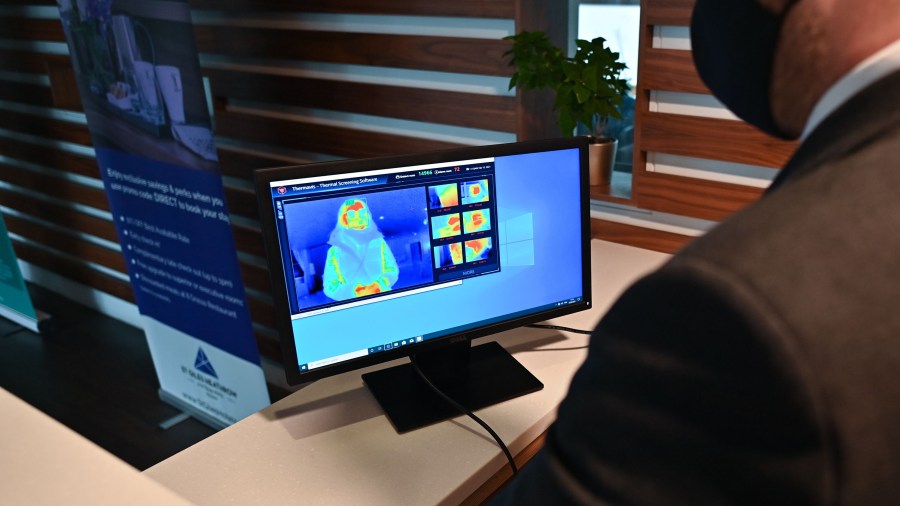
At the beginning of the pandemic, almost exactly this time last year, we heard a lot of promises about the types of technology that could help us stop the spread of the disease. One of those tech miracles was thermal cameras — devices that could read someone’s temperature from a distance. Companies bought them in droves, thinking that installing them at the entrances of schools, airports or offices could stop sick people from entering.
But do they work, and did they ever? I spoke with Conor Healy, the government director at IPVM, a video-surveillance research firm. He recently co-authored a study on fever-scanning devices and said many have one large flaw. The following is an edited transcript of our conversation.

Conor Healy: We found that they’re inaccurate, but not just that they’re inaccurate. They’re inaccurate in a particular way. The fever cameras are taking a reading of a person’s surface temperature each time you get scanned, but they’re adjusting that reading before it gets shown to the user who is evaluating whether or not that person should enter a facility. And if the reading is quite low, they’ll adjust it up. If the reading is high, they’ll adjust it down. The upshot is that this results in reducing temperatures that should be reported as fevers to the normal range and reporting them as normal.
Molly Wood: I mean, you’re saying it really nicely. It sounds like what you’re saying is: These do nothing, and there’s no point in using them. I can’t imagine how that would ever produce an effect that would keep people safe, if what you were trying to do is keep people with fevers out of a building.
Healy: Yeah, well, I can’t imagine how it would keep people safe either. But it’s more than the fact that they’re just not detecting fevers, they’re actually actively telling people that their temperatures are normal.
Wood: What’s your understanding of why that software exists and the readings are getting revised? Are they compensating for low-quality sensors?
Healy: In my opinion, they are making up for poor performance, as you suggested. In many cases, they’re using low-resolution sensors, and that’s part of it. But comprehensively, when you look at the design, manufacturing, implementation and marketing of these devices, there are so many pieces that get in the way of doing accurate temperature screening with a thermal camera. And this compensating algorithm creates an appearance of normal function. And nobody investigates a normal temperature, or considers it odd that somebody’s temperature would be normal when it’s reported by one of these devices. And so if they’re either poorly manufactured or not used in a way that’s consistent with how they should be used in order to take accurate readings, the compensating algorithm might make up for that and make everything seem like it’s working just fine.
Wood: What do the companies say? For example, it seems like at least one of them told you it was to make up for a factor like people coming into a building from the hot sun.
Healy: Yeah, some companies have used that justification. I mean, the thing is that somebody is coming in after being in the hot sun, what the [Food and Drug Administration] says and what the [International Electrotechnical Commission] says, which is an international group of scientists that convened and came up with guidelines for human temperature screening with thermal cameras, what they say is that people should wait inside for 15 minutes at room temperature before being screened for exactly that reason: that coming in from a hot environment or cold environment will affect the reading that you have. So the correct solution to that is not to just simply adjust the readings so that they’re more normal.
Wood: You also noted that some of the companies selling these scanners only got into business in the past year, likely because of COVID-19. Is that a cause for concern?
Healy: Yeah, absolutely. What’s quite typical is that they are actually not manufacturing them. They’re buying them from someone else and relabeling them. That is a big concern. Many of these smaller companies would not and have not been able to answer questions about why their devices might even have a compensating algorithm, because they may well not know.
Wood: I mean, when there’s something like this, there’s always a rush to sort of security theater. And I wonder if over the past year have you seen any use of this technology that’s actually been successful that we know of and helping slow the spread of COVID-19?
Healy: In general, no. I can’t think of an example to give you. I’m sure that there are setups out there. I’m sure that there are many that are done correctly, and that are potentially accurate enough for human screening, but they would be quite rare.
Wood: Should there be some rules? Like, if these are being touted as medical devices or medical-grade devices that can keep people safe going back to work or school, should there be more stringent requirements?
Healy: There are rules. And those rules were essentially waived. The FDA said, “We’re not going to object to new devices coming onto the market because we don’t want to impede the supply.” It’s been almost a year since they said that. There is plenty of supply now. And the rule should be put back into place.
Wood: Are there FDA-approved scanners that work?
Healy: There are ones that work in the sense they don’t have a compensating algorithm, and they’ll work if you use them correctly. So, yes and no. And the no part of that question is that people, even many of the people selling these devices, really just don’t appreciate how complicated it is to use them to take human temperatures. You need to control the humidity level in the screening area, the ambient temperature and the sources of light, especially the sun, reflective surfaces. These cameras generally run into $10,000 to $12,000, and the FDA-cleared handheld thermometer that we use in our study goes for anywhere from $40 to $150.

Related links: More insight from Molly Wood
The FDA on March 4 sent warning letters to companies that might be selling unauthorized devices. One thing I did find interesting is that the letter included a quote from the agency’s head of device-quality evaluation, who said that if a device can detect an elevated temperature, it “can be an important risk management tool during the pandemic when used properly.” However, lots of COVID-19 spread happens from people who aren’t showing any symptoms. Researchers say even if they’re used correctly and are accurate, temperature guns alone are pretty insufficient when it comes to keeping an area safe, because they certainly aren’t going to catch everyone who’s infected. And given all the problems with using these devices correctly or tracking which ones aren’t FDA-cleared at all, I have to say it’s still surprising to hear the FDA determine that there’s any reason for this ongoing health security theater, which even Dr. Anthony Fauci said last August he doesn’t even bother with when he’s going to the White House or the National Institutes of Health.
And other doctors have said the thermometers can contribute to a false sense of security, leading people to think everything is just fine in the place they just walked into, so I’m not sure where the idea that they’re good risk management is still coming from. This is, of course, the same FDA that only just this week moved to streamline approval for at-home COVID-19 tests, which could help catch asymptomatic infections before people even leave the house and have someone wave a useless chunk of metal at them before letting them into the bar or hair salon. Health experts have been arguing for almost the entire duration of the pandemic that widespread cheap and easy access to testing is the best possible way to keep the spread under control, followed closely by wearing a damn mask, and yes, making sure it goes over your nose.
The future of this podcast starts with you.
Every day, the “Marketplace Tech” team demystifies the digital economy with stories that explore more than just Big Tech. We’re committed to covering topics that matter to you and the world around us, diving deep into how technology intersects with climate change, inequity, and disinformation.
As part of a nonprofit newsroom, we’re counting on listeners like you to keep this public service paywall-free and available to all.
Support “Marketplace Tech” in any amount today and become a partner in our mission.


















