
COVID hot spots are pointing the way for future health care development plans
COVID hot spots are pointing the way for future health care development plans

The southeast suburbs of Nashville stood out on COVID-19 heat maps in the early months of the pandemic. Two zip codes accounted for 40% of all the city’s cases, according to the city’s coronavirus task force.
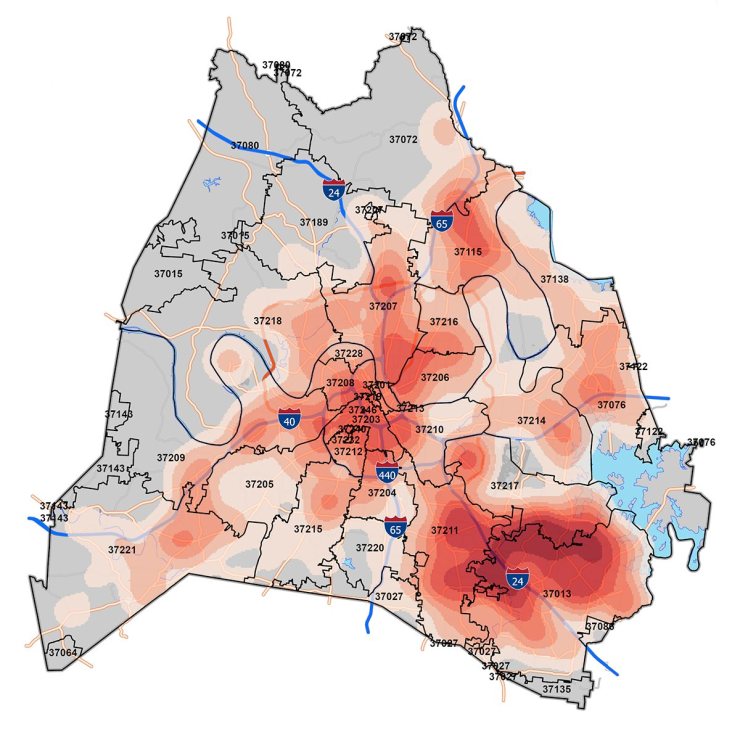
It just so happens that the area known as Antioch is relatively far from the city’s medical district. So now, the biggest hospital in the region is moving in.
“Thank you, thank you, thank you,” local Council Member Joy Styles said to officials from Vanderbilt University Medical Center at an announcement in March. “We are all so grateful.”
Behind Styles sat a largely vacant shopping mall. Vanderbilt plans to turn it into a mammoth medical office, and the medical center announcement cites the high rates of COVID as one primary reason for the expansion.
There were places in the country where COVID hit particularly hard and those hotspots revealed some of the gaps in health care. Now, some health care providers are expanding and using the lessons they have learned during the pandemic.
The Vanderbilt development is located at the center of some of the most diverse neighborhoods in Tennessee. Many residents are Black and Latino and there are refugees who’ve moved there from around the globe.
Dr. Consuelo Wilkins, who oversees health equity at Vanderbilt, said residents are more likely to live in multi-generational households and have hands-on jobs that don’t allow for telecommuting.
“These are people that we were saying, early on, were the essential workers,” she said.
Even before the pandemic, there was evidence this area was underserved, with fewer people who have health insurance.
“But the spotlight that a lot of people have talked about being shown on this is something COVID brought, that’s really hard to ignore,” Wilkins said.
COVID-19 isn’t the only reason projects are moving forward. But state regulatory filings, known as a certificates of need, show the pandemic is providing additional justification for many expansion applications in Tennessee, Mississippi and beyond.
In some cases, states are encouraging COVID-related expansions. In recent weeks, Tennessee set aside the last of its federal stimulus funding — about $230 million — in part to help hospitals in one-time hotspots to build more intensive care units.
The pandemic has even revived interest in reopening rural hospitals, abandoned for years.
“If anything, this whole pandemic has taught us there is greater need than ever before,” said Dr. Aley Hamadani, an emergency physician who worked in the small hospital in Parsons, Tennessee. It closed just after the pandemic began.
Hamadani now runs the ER in a neighboring county for Braden Health, which is attempting to reopen his old hospital and others. Some are in counties with COVID death rates that are 50% higher than the national average of roughly 1.2%
The pre-pandemic assumption that rural residents who lost their hospitals could just drive to bigger cities turned out to be wrong, Hamadani said. During COVID surges, even urban medical centers were overwhelmed.
“There’s no beds anywhere,” he said. “And what are patients supposed to do? Just die on the street?”
But the aspiration to meet needs highlighted by COVID is coming up against another trend: Health systems are having trouble finding nurses to staff their existing operations.
So in yet another way, the pandemic is beginning to shape growth.
The Ascension health system’s main hospital in Nashville is finishing up a $300 million critical care and surgical tower. Plans were overhauled midstream with an eye to making life easier on nurses — in hopes of improving recruitment and retention — by adding basic amenities, such as locker rooms with showers and supply closets for nurses closer to patient rooms to cut down walking.
“Not being cognizant of the fact that they have additional needs that we can plan for and intentionally deliver on seems shortsighted,” said Dr. Shubhada Jagasia, the hospital CEO.
Broadly, there’s a recognition that COVID didn’t create new needs so much as it revealed those that have existed beneath the surface and will remain even if the pandemic fades away.
There’s a lot happening in the world. Through it all, Marketplace is here for you.
You rely on Marketplace to break down the world’s events and tell you how it affects you in a fact-based, approachable way. We rely on your financial support to keep making that possible.
Your donation today powers the independent journalism that you rely on. For just $5/month, you can help sustain Marketplace so we can keep reporting on the things that matter to you.


















