Rethinking hospital readmissions
Share Now on:
Rethinking hospital readmissions
Kai Ryssdal: The list of reasons health care costs in this country are so high is a long one. We’re not going to rehash all of them here, but we are going to highlight one that is — in most cases — totally avoidable: Hospital readmissions.
Say you’re a senior citizen on Medicare and you go to the hospital — 1 out of every 5 times, that is, 20 percent of the time, you’ll end up back in the hospital before the month is out. That gets expensive in a hurry. So under the health care reform law, starting this October, hospitals with too many readmissions are going to get fined. Which is forcing them to look at what’s happening outside their own doors and to go beyond just doctors and nurses.
From the Marketplace Health Desk at WHYY in Philadelphia, Gregory Warner has more.
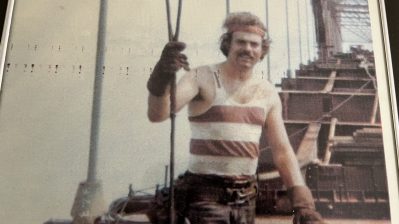
Gregory Warner: When he came back from Vietnam, Joe Francis discovered that all the money he’d sent back home for his education had been spent by his mother. When he finally got his degree in engineering — and he was the first in his family to go to college — his mom said what she always said when he read a book or got a good grade.
Joe Francis: She’d use an expression, “You ain’t doing nothing, but showing off.” And I never had her support.
When Joe Francis lost his job five years ago at age 56, he found himself completely alone, without family, estranged from his son, his brother and sister dead. And Joe, who’s a lifetime smoker, became compulsive about his habit. He has emphysema and asthma, so when he smokes his lungs spasm and he has to be rushed to the hospital.
Francis: I went to the emergency so much, the doctors knew my name. They’d say, ‘Mr. Francis you’re back again. You know you’re killing yourself.’ And in the back of my mind I wanted to. I would leave the hospital, I’d buy three packs of cigarettes and see how fast I can smoke ’em up. I was literally trying to kill myself.
Warner: Did you know you were trying to kill yourself?
Francis: I did. Because I knew before these three packs of cigarettes up. I’m gonna call the EMT. I’d made sure that door was unlocked. I made it easier for them to get me.
Warner: If you were trying to kill yourself, why did you call the EMT?
Francis: Well, I didn’t want to die alone. A couple people in here died in their apartments and they found them. I didn’t want to be alone when I died.
All those hospital visits, oxygen tanks, the X-rays, the MRIs, the CAT scans — the Veterans Administration picked up the tab for all of it.
Francis: It cost them a lot.
Dr. Shreya Kangovi is an internist at the Hospital of the University of Pennsylvania. She says every doctor knows these patients.
Shreya Kangovi: We just focus on the medical issues and spend tens of thousands of dollars ordering MRIs, titrating every milligram of their blood pressure medications, and on the day of discharge, buh-bye!
And that buh-bye costs taxpayers. Let’s take Medicare — the government program for seniors. It spends $17 billion a year on patients that cycle in and out of the hospital more than once a month. And there’s no incentive for hospitals to stop those patients from returning.
Kangovi: Hospitals have nothing to lose with readmissions, they are paid for admissions and keeping their hospital beds full.
Hospitals have always said there’s nothing they can do to change how people behave once they leave the hopsital. But starting this October that excuse won’t wash any more. As part of the new health care law, hospitals will face hefty fines for allowing too many readmissions. At Penn, Dr. Kangovi launched a program that focuses on the five poorest zip codes in Philadelphia — responsible for 85 percent of readmissions in the city. That’s how Mary White first met Joe Francis, the engineer we met before.
Mary White: When I first met Mr. Francis he was in Presbyterian Hospital. He was hooked up to oxygen, could barely breathe, could barely walk. So I introduced myself. I told him I was a community health worker.
A community health worker is not a nurse. It’s not a home aide. It’s defined as someone who has the same background as her clients. Mary White and Joe Francis are both black, they both grew up in Philly. They’re almost the same age. Both have had health problems. They could relate.
Francis: She said, ‘I’m going with you to your appointments.’ She caught the bus. And I said wow, she kept her word! When I got out of the hospital you said well Joe you’re doing better, you’re walking down the street like you’re a young men! Remember you told me? And I said, I actually have somebody standing by my side. And in my mind I said I’m gonna get well for you.
Warner: How long did you guys spend, together, working together?
Francis: About two weeks!
White: It was two weeks.
Within two weeks, Joe started going to a community senior center that Mary introduced him to. A month later he was teaching classes there — one in drums, the other in computers. Those two weeks did what six years of therapy and no-smoking programs and nicotine patches couldn’t do.
Francis: Mary had a lot to do with me stop smoking. It was just her heart and the generosity she showed that gave me confidence in myself.
And Joe hasn’t been back to the hospital since. Of course, not all of Mary’s clients have such a radical transformation. Readmission is a complex problem rooted in poverty. But there is something about Mary. Here’s Dr. Kangovi.
Kangovi: In the sociology literature, these people are referred to as natural helpers. They’re the type of people that will be at a neighbor’s bedside whether they’re being paid to or not.
So with Mary White, the morning that I met up with her, she’d woken up early just to cook breakfast for an injured neighbor.
White: So that was before work.
A couple of days before, while waiting for her ride home from work…
White: You know, people watching after I got off from the job.
She spotted a woman with one leg struggling to carry her suitcase and crutches. Mary helped her.
White: And so I filed her out to the car. And she said, ‘Thank you, that was very sweet.’ Then another lady, she looked like she was a stroke victim and I said, ‘Do you need help walking to you car?’ And she said, ‘No, I’ll be all right,’ then she turned around and says, ‘I really could use that help.’ So I walked her out to her car! And that was just while I was waiting to go home myself! So that’s, that’s just a part of me. So, just a natural helper!
Warner: That’s just a natural helper.
White: Yes.
Warner: Because you saw them.
White: Yes. Because I saw them.
The hope is you pay this kind of person to lower health care costs? You might actually get somewhere.
In Philadelphia, I’m Gregory Warner for Marketplace.
There’s a lot happening in the world. Through it all, Marketplace is here for you.
You rely on Marketplace to break down the world’s events and tell you how it affects you in a fact-based, approachable way. We rely on your financial support to keep making that possible.
Your donation today powers the independent journalism that you rely on. For just $5/month, you can help sustain Marketplace so we can keep reporting on the things that matter to you.